Attilio
Cavezzi
Vascular Unit , Clinic "Stella Maris"
S. Benedetto del Tronto (AP), Italy
Varicose vein treatment
may be of surgical nature when varices arise from incontinence of the long saphenous
vein (LSV), short saphenous vein (SSV), anterior saphenous vein (ASV) or in
cases of post-surgery recurrences. Besides the surgical approach, ultrasound
guided sclerotherapy (UGS) has conquered new horizons in the last few years.
In fact UGS is proposed by many phlebologists as the first choice for SSV and
recurrent varicose veins; this attitude is justified in our experience, especially
after the recent introduction of the sclerosing foam which seems to enhance
the power of UGS.
However it has to be remarked that varicose vein surgery has improved its cosmetic
results, becoming less invasive, more conservative, finally competing with sclerotherapy
even for the treatment of smaller varicosities (tributaries of LSV and SSV,
and even in case of reticular varices).
According to our experience the integration of these two therapeutic methods
may constitute the best treatment for varicose vein disease. Whichever therapy
is chosen, it should be modulated according to the morphologic and functional
findings of the pathologic limb.
The correct therapeutic approach should rely on an accurate diagnosis, which
requires the investigation of the patient by means of duplex scanner or, better,
by means of colour-flow duplex imaging (CFDI). An adequate diagnosis may be
achieved by using the CFDI tool, obtaining both a reliable guide for any therapeutic
step and a formidable non-invasive method to follow-up the treated limb. In
fact duplex technology, as the main protagonist of a true revolution in phlebology,
is definitively creating a sort of watershed among all the actual numerous (too
numerous..) ways to treat superficial venous insufficiency.
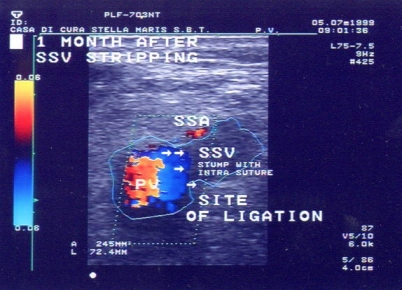
Within the surgical treatment for varicose veins, in cases of LSV or SSV incompetence
the stripping technique still represents the choice intervention. New forms
of surgical treatment are enriching the scientific panorama in this field (CHIVA,
above all), but future studies (a few of them are already available) will provide
eventual evidence of good results, permitting a serene comparison and integration
among the methods.
Old and new studies have depicted the short stripping or, better, the segmental
stripping of the incompetent saphenous tract, as the ideal surgical approach
. In fact the reflux (or retrograde flow) is generally limited within LSV and
SSV: nearly all the patients (97% in a recent study of ours) have no reflux
in the lower third of the leg. Sparing the healthy segment of LSV or SSV is
becoming mandatory, on the basis of all the information provided pre-operatively
by duplex or CFDI mapping. A blind groin (popliteal)-to-ankle stripping has
definitively become obsolete and useless in most cases, permitting the avoidance
of the typical complications related to the long stripping.
Among the stripping techniques, the invagination one is the most respectful
of the integrity of the peri-saphenous nerves and lymphatics, having also very
good aesthetic characteristics and a favorable haemostasis . We usually perform
the invagination technique by means of a plastic disposable stripper, more rarely
according to the PIN stripping technique.
With regard to the first part of saphenous stripping , that is the crossectomy
(flush ligation of the saphenous junction, at femoral or popliteal level, with
disconnection of all the tributaries of the saphenous junction), the frequent
CFDI or duplex finding of the saphenous stem incompetence in presence of the
continent saphenous junction should be highlighted: in these cases no reflux
comes from the deep venous system across the terminal valve of LSV or SSV.
This kind of remark is due to the improving capability and the extended use
of instrumental diagnostics. In fact patients are more frequently being investigated
pre-operatively by means of duplex scanner or CFDI, which allows a finer diagnosis;
moreover patients are requiring operations more precociously than in the past:
if saphenous disease starts from the periphery in the vast majority of the cases,
as it is argued from a few recent studies, the earlier the patient comes for
the vascular investigation, the more the junction is competent...
When facing such a haemodynamic condition (varicose veins arising from saphenous
incontinence, without junction incompetence), the surgical attitude may be more
or less conservative; sometimes it could be possible to perform the CHIVA 2
technique, which is the ligation of the varicose tributary of LSV or SSV, just
flush with the saphenous stem, excising the varices by hook phlebectomy. By
doing so it is possible to avoid any surgical procedure on the saphenous junction
and stem, but only in selective indications. In the vast majority of CHIVA 2
treated limbs, the abolition of the reflux will be possible in the vast majority
of the patient, furthermore most of the remaining patients will have a re-enter
of the saphenous retrograde flow into a perforator, and in the long term only
a few cases should re-operation be expected. Future studies should confirm this
attitude, but preliminary results seem encouraging.
The typical completion of saphenous stripping relies upon mini-incisions phlebectomy
(Muller's technique), which represents a surgical approach with great cosmetic
requisites and great possibility of radicalization.
Phlebectomy method is based on 1-2 mm incisions, which we perform sometimes
by 18 Gauge needle, obtaining no scar just 7 days post-operatively; phlebectomy
provides the extensive avulsion of large varices, with relevant results at long-term
follow-up (when correctly executed after the elimination of main saphenous refluxes).
We prefer to perform this method separately, when indicated, or contextually
at the stripping operation, relying on phlebectomy for saphenous tributaries
or inter-saphenous branches; it is very rarely used for LSV or SSV stems.
Technical and tactical aspects of perforating veins (PV) surgery have been widely
debated in the last few years. PV have recently been re-evaluated with regards
to their pathogenic role: Bjordal, Bassi, Tibbs and Franceschi have progressively
updated our knowledge, clarifying that most of them have a re-entry role in
the leg (in primary varicose veins).
In our practice PV are avulsed (partly) by phlebectomy, sometimes using the
torsion-rupture technique, avoiding any ligation; extra-saphenous thigh PV or
very large PV may be ligated in selective, rare cases. The vast majority of
the peripheral (leg) PV allow the re-entry of the saphenous retrograde flow
into the deep venous system . When a bi-directional flow is present, the main
inward diastolic flow is evident and in these cases the surgical procedure could
be mini-invasive. SEPS or subfascial blind ligation of PV in primary varicose
veins are frankly questionable almost in all the patients. Even the absolute
abstention from any surgery seem to provide good short-term results in cases
of re-entry perforators located in the lower part of the leg...
As far as surgery for varicose veins is concerned, the role of local anesthesia
is fundamental; local anaesthesia by subcutaneous infiltration is the main protagonist
of the conversion from the traditional, expensive hospital-surgery to the cheap
and mini-invasive day-surgery for varices, improving patients' compliance remarkably.
In our experience all patients deambulate 1-2 hours after the intervention,
and more than 95% of them only need a 6-12 hours hospitalization, returning
home (where most of their daily activities are permitted) in the same day of
the saphenous stripping / phlebectomy operation. This result is made possible
by a pure local anaesthesia technique (0,25%-0,4% mepivacaine), rarely assisted
by a 30 second sedation by propofol i.v.
Finally elastic compression represents a necessary and mandatory technique to
manage the post-operative period. We use eccentric positive (by means of different
pads), multi-layered elastic compression and our preferred means of compression
are the adhesive-bandage or, recently, the specific STRUVA ® 35 mmHg elastic
stocking; these devices contribute to significantly reducing all the typical
complications related to these operations, optimizing the cosmetic and functional
results.
This kind of surgery for varicose veins on an outpatient basis results in a
high degree of safety, mini-invasiveness and cost-effectiveness, gaining the
favour of the vast majority of patients . This integrated and holistic approach
must include reliable diagnostics, accurate anesthesiology technique, careful
surgical procedure and experienced compression use; all of these aspects constitute
a demanding attitude for the physician, but this multi-faceted approach has
become necessary in order to achieve the right functional and cosmetic outcomes,
respecting as well as possible the limb venous drainage.