ULTRASONIC ASSESSMENT OF AMBULATORY VENOUS PRESSURE
IN PRIMARY VENOUS INSUFFICIENCY
Paolo Zamboni, Diego Quaglio, Caterina Cisno, Federica Marchetti, Maurizio Giacometti, Maria G. Marcellino
Department of Surgery and Vascular Laboratory
University of Ferrara (Italy)
Address correspondence to:
Paolo Zamboni, MD
Department of Surgery
University of Ferrara
44100 Ferrara (Italy)
telefax: +39-532-249358, telephone: +39-532-236525
E-mail: zmp@dns.unife.it
Short title: Noninvasive assessment of AVP
Presented at the World Congress of the Union International de Phlebologie, Sidney, September 6-11, 1998.
ABSTRACT
Purpose: in spite of its invasiveness, ambulatory venous pressure (AVP) is widely considered the gold standard measurement of venous function. We studied a technique for noninvasive ultrasonographic AVP determination in primary venous insufficiency of the lower limbs.
Methods : a linear relationship between venous pressure (measured by echo-guided venous puncture) and diameter (measured by transvers access duplex imaging) was preliminarly demonstrated with multiple measurements in different conditions (supine, sitting, standing, and Trendelemburg positions, after exercise with and without cuff occlusion) in a saphenous tract at the thigh of 82 limbs in which reflux had been priorly demonstrated. Then, AVP was measured in another group of 44 patients with demonstrated superficial venous incompetence, both with and without proximal occlusion, using again the same invasive method and a new noninvasive technique. The latter consisted in the construction of a linear diameter/pressure curve obtained after saphenous diameter (by high resolution sonography) and noninvasive pressure (using hydrostatic values) determinations in the sitting and standing positions. Further measurement of saphenous diameter after standardized exercise permits extrapolation of the AVP values from the curve. Non invasive calculations were also made by the means of the soft-ware Venometer and compared with manual assessment.
Results: Linear regression analysis demonstrates that: a) starting from 20 mm Hg, the pressure/diameter relationship of the incompetent greater saphenous vein is linear; b) AVP values derived invasively and noninvasively are significantly correlated (r=0.73 and P < 0.0001 for AVP derived without occlusion, r=0.73 and P < 0.0001 for values recorded with occlusion). Assessment by Venometer as compared to manual calculation showed a high degree of correlation (r=0.98, P < 0.0001).
Conclusions: The proposed technique appears able to reliably assess noninvasively AVP values in primary venous incompetence. In addition, it can be performed by means of an equipment widely used for vascular investigations.
Finally, Venometer allows an easy and rapid estrapolation of AVP values.
Key Words: Ambulatory Venous Pressure, Venous Function, Ultrasonography.
Venous function of the lower limbs has proved to be a difficult entity to quantify. Many tests have been developed in an attempt to separate normal from abnormal function, including ambulatory venous pressure (AVP), foot volumetry, photoplethysmography, air plethysmography. Unfortunately, none of these methods can completely categorize patients and limbs by clinical severity of the disease (1-10).
The fall of venous pressure occurring with exercise represents the functional reserve of the venous system of the lower limbs and closely correlates with the clinical class of chronic venous insufficiency. Although some overlap exists between AVP values obtained in either healthy or insufficient veins of the lower limbs, such a measure is widely considered the gold standard in the evaluation of venous function (1-6, 8, 10). Unfortunately, AVP is measured invasively, whereas an ideal test should be noninvasive and easily repeatable.
We postulated that the relationship between vein diameter and pressure is linear in the incompetent saphenous vein after completion of the filling phase. If this is true, a linear diameter/pressure curve could be noninvasively derived from duplex scanning measurements of vein diameter and linear measurements of the distance between the heart and the point of saphenous diameter measurement (multiplied by a constant to obtain the hydrostatic pressure) in two different hydrostatic conditions: sitting and standing. The aims of this study were: a) to demonstrate the linearity of the diameter/pressure relationship after the filling phase in the greater saphenous vein (GSV) of patients affected by primary venous insufficiency; and b) to assess whether a close correlation exists between the standard intravenous method (control method) and the new, non invasive, ultrasonographic procedure (experimental technique) of AVP determination in such patients.
METHODS
Phase 1 - Development of pressure/diameter relationship.
Eighty-two limbs in 82 patients (52 female, 30 male, mean age 54 years) who were referred to our vascular laboratory for chronic venous insufficiency due to primary venous incompetence had their diagnosis confirmed by clinical examination (positive Trendelemburg and Perthes tests), photoplethysmographic refilling time measurement (measurement of a refilling time less than 18 sec after exercise and its prolongation after placing a cuff at the superior third of the thigh were both considered criteria for diagnosis of superficial venous incompetence) (10), and duplex scanning examination (superficial vein incompetence was characterized by a reverse flow longer than 0.5 sec (22), detected at least in one saphenous segment when Doppler sample volume was placed, with an angle of 45 deg, at five different levels along the GSV and the sapheno-femoral junction, during manual calf squeezing in the standing patient; the manual squeezing manoeuvre was always performed by the same investigator (MGM).
The femoral and the popliteal vein, in addition to the sapheno-popliteal junction were also investigated.
The patients gave informed consent and the protocol was approved by the Ethical Committee of our Hospital.
The patients were classified according to the new CEAP criteria of chronic venous insufficiency (11). The clinical class, C, ranged from 2 to 6 and more specifically: 34 patients presenting with simple varicose veins (C2), 23 patients with oedema (C3), 15 with lipodermatosclerosis and/or other skin changes (C4), 6 with healed ulcer (C5) and 4 with active ulcer (C6). The etiology, E, was always primary. The anatomical distribution of cases, A, was in the GSV above the knee in 23 cases, above and below the knee in 59 cases. Perforators were incompetent at the thigh in 19 cases and at the calf in 82 cases. Coexisting short saphenous vein and femoral vein incompetence was found in 7 and 5 cases, respectively, the latter finding always corresponding to patients in clinical class 5 or 6. Finally the pathophysiology of chronic venous insufficiency, P, derived from reflux in all cases. The following algorithm describes the considered patients: C2-6/s, Ep, As2-3-4/d 11/p17-18, Pr.
All the measurements were performed between 8 and 10 AM at the same temperature (23°), just before surgery was performed for correction of chronic venous insufficiency.
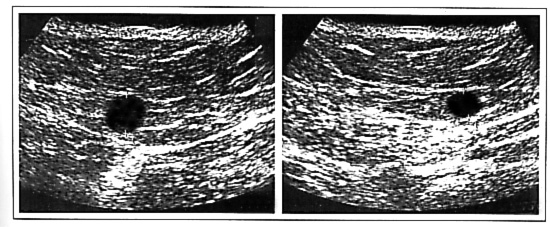
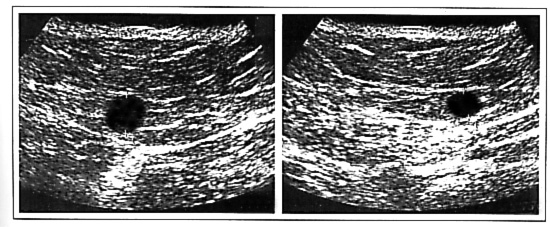
The values of diameter were measured by duplex scanning (AU 530, 7.5-10 MHz, Ansaldo, Italy) in a saphenous tract between the inferior third of the thigh and the superior third of the leg, in which we previously detected reflux. The so-called saphenous eye obtainable in the transverse access duplex imaging of the internal thigh was used as echographic marker for precise GSV identification (12-15). The ultrasonic beam was directed toward a rectilinear and non dilated part of this saphenous tract. In applying the probe against the cutaneous surface, we used the minimal pressure able to guarantee a satisfactory saphenous vein imaging, while avoiding undesirable compression that could have modified vein diameter assessment. This was easily obtained in every case, since vein compression is clearly visible on the ultrasound image. In measuring diameter we preferred the axis perpendicular to the skin, in the transversal scan (Fig. 1): it reflects the dimensional changes of the cross-sectional area, whereas the axis parallel to the cutaneous surface depends more on the flattening of the saphenous vein (16).
All saphenous pressures were intravenously recorded in the precise site previously measured by duplex, using a catheter-transducer (1290 A, Hewlett-Packard, USA). The puncture was performed under ultrasonic guide, using the above illustrated criteria for saphenous vein localization.
For each limb, seven diameter-pressure pairs of values were measured: in the supine position, in the sitting position, in the standing position, after exercise (ten tip-toe movements) performed without a cuff, after exercise performed with a cuff placed at the superior third of the thigh, and in two Trendelemburg positions (leg raised at -30° and -45 deg using a graduated bed). In the last condition we obtained only 12 pairs of values, due to the frequent impossibility of obtaining a reliable diameter measurement in a collapsed saphenous vein.
Phase 2 - Comparison of experimental technique to control method of AVP determination. Experimentation of automatic calculations by the means of Venometer.
Forty-four limbs in 32 patients (25 female, 7 male, mean age 46 years) who were referred to our vascular laboratory for primary superficial venous incompetence had their diagnosis confirmed by clinical examination, photoplethysmographic refilling time measurement, and duplex scanning examination, in accordance to the above illustrated criteria. The patients gave informed consent and the protocol was approved by the Ethical Committee of our Hospital.
According to the CEAP criteria of chronic venous insufficiency, the clinical class, C, ranged from 2 to 3 (24 limbs affected by symptomatic varicose veins (C2s), and 20 limbs affected by symptomatic varicose veins with oedema (C3s). The etiology, E, was always primary. The anatomical distribution of cases, A, was in the long saphenous vein above the knee in 13 cases, above and below the knee in 31 cases. Perforators were incompetent at the thigh in 11 cases and at the calf in 39 cases. Finally the pathophysiology of chronic venous insufficiency, P, derived from reflux in all cases. The following algorithm describes the considered patients: C2-3/s, Ep, As2-3/p17-18, Pr.
Methods of AVP determination.
Measurements were obtained from two different methods performed on the same occasion by two different investigators, blinded to the other's result.
The experimental technique is a non invasive method for in vivo clinical measurement of saphenous AVP. The control method is the standard intravenous assessment (AVP) (1-6).
Experimental technique. In order to extrapolate AVP values, a diameter/pressure curve of the saphenous vein was constructed.
Diameter and pressure were first measured in two different hydrostatic positions: sitting and standing.
The two values of diameter (D1, D2) were measured by duplex scanning (AU 530, 7.5-10 MHz, Ansaldo, Italy) in a saphenous tract of the thigh in which reflux was previously detected, in accordance with the above illustrated criteria.
P1-2 is the pressure of the hydrostatic column, i.e. the distance between the heart level and the point of saphenous diameter measurement in quiet standing (P1) and in sitting position (P2) according to the formula P = r x g x h (17). At 37 °C and with an ambient pressure of 1 atm, r x g can be considered a constant. Consequently, P1-2 (mm Hg) is equal to 0,7723 x h, where h is the distance (in cm) between the heart level and the point of measurement.
We considered the heart level to be at the third interspace at the sternum, which Cunningham described as the level of the middle of the right auricle (18).
Zero point of the curve was arbitrarily considered a pressure value of 20 mmHg (P0). This is the lowest level of pressure from which the saphenous diameter/pressure relationship at the thigh can be approximated to a straight line. This was previously determined in Phase 1 of the study (see Results section). Hence, <<<<<<<the axes intersection was set to 20 mm Hg in order to shift the reference system to the minimum level from which the diameter/pressure relationship was demonstrated to be linear (Fig. 3).
AVP was then derived after 10 consecutive tip-toe movements, both with and without echo-guided external finger occlusion of the proximal saphenous vein (2). Using ultrasound imaging, it was always very easy to check the site and the completeness of the occlusion. We outlined the point in which the measurement was previously assessed, and maintained the duplex probe on the skin during standard exercise. When the last movement was finished, the saphenous eye image was freezed exactly when the heels touched down to obtain the change in diameter after exercise (Fig. 1).
The two values were plotted on the diameter/pressure curve previously created, allowing the extrapolation of two AVP values, respectively with and without sapheno-femoral reflux elimination, as shown in Figure 3.
Control method. The control method was always performed after the experimental method to avoid a possible influence (vasospasm) of venous puncture on subsequent determinations. All saphenous pressures were intravenously recorded in the precise site previously used for the experimental method, using a catheter-transducer (1290 A, Hewlett-Packard, USA). The puncture was performed under ultrasonic guide, using the above illustrated criteria for saphenous vein localization.. We derived AVP, after standardized exercise, both with and without occlusion effect (1-6).
Soft-ware experimentation.
The soft-ware Venometer (OnLine, Ferrara - Italy: www.4net.com/business/online) allows CEAP classification as well as the automatic assessment of AVP. Calculations and curves were obtained simply entering in the personal computer the four values of diameter (sitting, standing, after exercise with and without saphenous occlusion) and the two distances in cm between the heart and the point of measurement The automatic calculation were compared to the manual one.
Statistical analysis.
The linearity of the pressure/diameter relationship in each individual patient above 20 mm Hg (phase 1), the relationship between AVP values invasively and non invasively assessed and manual and automatic assessment (phase 2) were calculated and tested for significance by linear regression analysis. Linear correlation for non parametric data (Spearman rank correlation test) was also determined with 95% confidence interval when appropriate.
RESULTS
Phase 1 - Development of a pressure/diameter relationship.
The results of the pressure/diameter measurements performed in the first group of 82 patients affected by primary chronic venous insufficiency, always involving the GSV, in 7 different hemodynamic conditions (supine, sitting, standing, after exercise, after exercise with cuff occlusion of the GSV, after leg elevation at -30 deg, and at -45 deg) are plotted in Fig. 2. It appears that the measurements are characterized by little increases in pressure and significant increases in diameter for values below 20 mm Hg. Above this value, the pressure/diameter relationship appears to be linear.
The linearity of the diameter/pressure relationship above 20 mm Hg was checked in each individual patient by calculating the statistical significance and the explained variance of the linear correlation among the multiple diameter/pressure pairs of each subject in which pressure values equalled or exceeded 20 mm Hg. All subjects had at least 3 pairs, and 63 subjects at least 4 pairs of values which satisfied this condition. While statistical significance was always high (P < 0.001), the explained variance (r2) of the experimental data ranged from a minimum of 64 to a maximum of 98 (on average 88), which demonstrates the correctness of the assumption of linearity also in the individual patients. The severity of venous insufficiency did not appear to influence such linearity, as indicated by the lack of any statistical difference in explained variance between class 2-3 and class 4-6.
Phase 2 - Comparison of experimental technique to control method of AVP determination. Experimentation of automatic calculations by the means of Venometer.
Four patients were excluded from evaluation because of unsatisfactory back-flow after puncture and vein waveform on the monitor.
The mean value of AVP invasively assessed without proximal saphenous occlusion was 48.2 ± 9.1 mmHg (range: 29-71), while the mean non invasive measure was 47.4 ± 10.1 (31-71); with occlusion we recorded 29 ± 7.6 (20-49) mmHg and 27.8 ± 6.9 (18-42), respectively .
Linear regression analysis demonstrated that AVP values derived invasively and non invasively were closely and significantly correlated (r=0.74 and P < 0.0001 for AVP derived without occlusion, r=0.73 and P < 0.0001 for values recorded with occlusion). The r value obtained with the Spearman rank correlation test was 0.73 with (95% confidence interval ranging from 0.53 to 0.85) and 0.67 without occlusion (95% confidence interval ranging from 0.45 to 0.82).
Finally, linear correlation test between the automatic assessment of non-invasive AVP by Venometer on one side and the manual estrapolation from the other, showed a high degree and a significant correlation (r=0.98, P < 0.0001).
DISCUSSION.
Duplex examination represents a great enhancement in venous diagnostics, allowing non invasive recognition of obstructed vein segments as well as reflux detection and quantification (19-22). Nevertheless we strongly believe that duplex scanning is still an underutilized tool in the assessment of venous disease. There is a lot of information that is usually left out, including measurement of vein diameter and its variation under postural and pressure changes (23-25).
The first main finding of our study is the demonstration of linearity, starting from a pressure value of 20 mm Hg, in the pressure/diameter relationship of the GSV of patients affected by primary venous insufficiency. This can be considered the first pathophysiologic demostration of the Law of the relationship between vein diameter and pressure in primary cases.
We know from classical physiology that the relationship between vein volume and pressure is characterized by a significant increase in volume with little change in pressure during the filling phase, in which the vein is distended by the increase in blood volume (25-29). In other words, during this first phase the pressure/volume relationship is not linear. Instead, during the distension phase following the filling phase, further increases in volume are proportionally reflected by pressure increases, so that linearity of the volume/pressure relationship in veins can be demonstrated starting from pressure values around 20 mmHg (27). On the other hand, after completion of the filling phase, vein diameter is geometrically related to vein volume (provided that vessel length is constant, volume equals area and area is 1/4 p x diameter) (26-29). This may explain our finding of a linear pressure/diameter relationship in the saphenous vein at the thigh, starting from 20 mmHg. Our patients were all affected by primary superficial venous insufficiency including all classes of clinical severity, but the presence of venous reflux did not appear to significantly affect the linearity of the above mentioned relationship. Instead, by shifting the ambulatory venous pressure toward values higher than normal, primary venous insufficiency may favour the occurrence of the hemodynamic conditions of vein distension at which the pressure/diameter relationship is linear. The linearity was maintained also in the five patients who had deep venous insufficiency coexistent with the superficial reflux, but this finding needs confirmation in a larger number of such patients.
Based on the results of the first phase of the study, we experimented a non-invasive technique for extrapolation of saphenous AVP values from a diameter/pressure curve. This can be obtained by a straight line drawn from the point of initial venous distension (20 mm Hg) and best approximating the two pressure/diameter values non invasively determined in hydrostatic conditions (sitting and standing) corresponding to linear measurements. When the heels touch the ground again at the end of the tip-toe exercise, the vein valves are open in telesystole exactly as in the postural conditions used to derive the diameter-pressure curve. Hence, the ultrasonographic measure of the saphenous diameter permits the extrapolation of an AVP value from the curve previously drawn.
Such measurements can be performed with and without saphenous vein occlusion, and in our study both values appeared to closely correlate with the corresponding intravenous determinations.
In clinical practice AVP is usually measured at the ankle. In contrast, we are proposing a non invasive method for AVP extrapolation at the thigh. In our opinion there are several reasons to prefer measurement at the thigh. First, when AVP is measured at the ankle in cases of superficial and / or coexisting superficial and deep insufficiency, the more significant hemodynamic modifications are obtainable by acting at the superior third of the thigh with a cuff, a finger or a tourniquet in order to eliminate saphenous vein reflux. This indicates that in such cases major hemodynamic changes occur at the thigh, even if the site of measurement is at the ankle. Furthermore, in our experience, larger diameters and constant B-Mode marker of the saphenous vein at the thigh ("saphenous eye") make diameter measurement easier and more precise at this level. Finally, in primary cases where the proximal saphenous segment is involved by reflux, the thigh represents an ideal window opened on the vein system of the lower limbs. If the system is able to empty with exercise, we can document the reduction in vein diameter just as in the Perthes test. In contrast, if the system is unable to satisfactory empty, due to impaired muscle pump function or whatever cause, we do not document a significant reduction in diameter (and, of course, of AVP since they are linearly related).
The proposed technique is simple, easily repeatable due to its non invasiveness, and it can be performed by means of an equipment widely used for vascular investigations. In this preliminary study, it has been applied exclusively to a saphenous segment of the thigh where reflux was previously demonstrated, and in patients affected by primary varicose veins. It should be interesting to verify this extrapolation in other segments, normal conditions and other venous diseases.
Finally, the obvious interest of a noninvasive method for ultrasonographic AVP assessment lead us to experiment a soft-ware for its rapid calculation in clinical practice. Venometer demonstrated to permit easy and precise non-invasive assessment of AVP.
REFERENCES
1) Pollack A.A., Wood E.H. "Venous pressure in the saphenous vein at the ankle in man during exercise and changes in posture" J. Appl. Phys. 1949; 1:649-662
2) Bjordal R.I. "Pressure patterns in the saphenous system in patients with venous leg ulcers" Acta Chir Scand 1971; 137:495-501
3) Hojensgard I.C., Sturup H. "Venous pressure in primary and postthrombotic varicose veins. A study of the statics and dynamics of the venous system of the lower extremity under pathological conditions" I. Acta Chir. Scand. 1949; 99:133-153
4) DeCamp P.T., Ward J.A., Ochsner A. "Ambulatory venous pressure studies in postphlebitic and other disease states" Surgery 1951; 29:365-380
5) Randhawa GK, Dhillon CS, Kistner RL, Ferris EB: Assessment of chronic venous insufficiency using dynamic venous pressure studies. Am.J.Surg. 1984; 148: 203-09
6) Nicolaides A.N., Zukowski A.J. "The value of dynamic venous pressure measurements" World J. Surg. 1986; 10:919-924
7) Thulesius O, Norgren L, GjoresJE:"Foot volumetry, a new method for objective assessment of oedema and venous function. Vasa 1973; 2:235-9.
8) Sarin S., Shields D.A., Scurr J.H., et al "Photoplethysmography: A valuable noninvasive tool in the assessment of venous dysfunction" J. Vasc. Surg. 16:154-162, 1992
9) Christopoulos D., Nicolaides A.N., Szendro G., Irvine A.T., Bull M.T., Eastcott H.G. "Air-plethysmography and the effect of elastic compression on venous hemodynamics of the leg" J Vasc Surg 1987; 5:148
10) Belcaro G., Christopoulos D., Nicolaides A.N. "Basic data related to normal and abnormal lower extremity hemodynamics" Ann Vasc Surg 1991; 5:306
11) Porter J.M., Moneta G.L. and the International Consensus Committee "Reporting standard in venous disease: an update" J. Vasc. Surg. 1995:21;635-45
12) Zamboni P. La chirurgia conservativa del sistema venoso superficiale, C.E.L.I - Gruppo Editoriale Faenza Editrice, Faenza 1996, pp.3-9.
13) Somjen G.M. Duplex anatomy of teleangiectasias as a guide to treatment. In Ambulatory treatment of venous disease, M.P. Goldmann and JJ. Bergan ed., Mosby Year Book - St. Louis 1996, pp. 29-30.
14) Lemasle P, Uhl JF, Lefebvre-Vilardebo M, Baud JM" Proposition d'une definition echographique de la grande saphene et des saphenes accessoires a l'etage crural" Phlebologie 1996; 3: 279-86
15) Thomson H: The surgical anatomy of the superficial and perforating veins of the lower limb. Ann RCS Eng, 1979; 61: 198-203
16) Van Cleef J.F. "Valves in varicose veins and external compression studied by angioscopy" Phlebology 1993; 8: 116-19.
17) Cromer A.H. "Physics for the Life Sciences" New York, Mc Graw Hill, 1977, pp136-45
18) Brash J.C., Jamieson E.B. "Cunningham's text book of anatomy" New York: Oxford University press, 1937, pp.1145
19) Sullivan E.D., Peter D.J., Cranley J.J. "Realtime B-mode venous ultrasound" J. Vasc. Surg. 1984;1:465-71
20) Killewich LA, Bedford GR, Beach KW, Strandness DEJ" Spontaneus lysis of deep venous thrombi: rate and outcome. J.Vasc.Surg. 1989; 9: 89-97
21) Vadeskis SN, Clarke GH, Nicolaides A.N "Quantification of venous reflux by means of duplex scanning" J. Vasc. Surg. 1989; 10: 670-77
22) Masuda E.M., Kistner R.L., Eklof B. "Prospective study of duplex scanning for venous reflux: comparison of Valsalva and pneumatic cuff techniques in the reverse Trendelemburg and standing positions" J.Vasc. Surg. 1994; 20: 711-20
23) Davies A.H., Magee T.R., Hayward J., Harris R., Baird R.N., Horrocks M. "Non-invasive methods of measuring venous compliance" Phlebology 1992;7:78-81
24) Zamboni P., Marcellino M.G., Portaluppi F., Manfredini R., Quaglio D., Liboni A. "The relationship between in vitro and in vivo venous compliance measurement" Int. Angiology 1996; 15: 149-52
25) Zamboni P., Marcellino M.G., Quaglio D., Vasquez G., Murgia A.P., Pisano L., Feo C. "A reliable noninvasive methods for venous compliance measurements" Phlebology 1995;10 suppl.1:277-9
26) Burton A "The relation of structure to function of the tissues of the wall of blood vessels" Physiol.Rev. 1954; 34: 619-26
27) Starling EH, Lovatt Evans C "Principles of Human Physiology" J.A. Livingston, London 1956; Italian Version, Piccin , Padova 1959, pp. 600-601.
28) Norgren L., Thulesius O "Pressure-volume characteristics of foot veins in normal cases and patients with venous insufficiency". Blood Vessels 1975; 12: 1-12.
29) Thulesius O. "Vein wall characteristics and valvular function in chronic venous insufficiency" Phlebology 1993; 8:94-98
FIGURE LEGENDS
Figure 1: The so called saphenous eye image in standing posture (left) and after exercise (right), which allows diameter measurement in the saphenous vein at the thigh. Diameter assessment was always obtained from transverse access duplex imaging by measuring the axis perpendicular to the skin. The proposed method allows a measurement of the Perthes test.